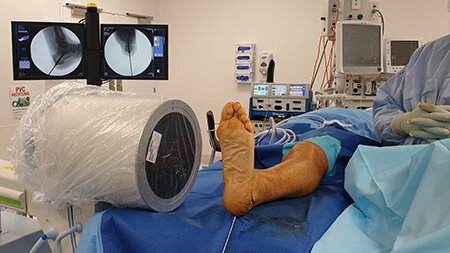
Flatfoot Surgery at Norwest Private Hospital Sydney
Flatfoot Surgery to restore the natural foot arch.
Reconstruction of the natural foot arch is the goal of a variety of surgical procedures to relieve pain, correct foot deformities, or restore function of the foot.
Flatfoot can be a debilitating condition where the normal arch of the foot is lost and continue to progressively worsen until pain and postural problems become apparent.
What is Flatfoot Surgery?
Flatfoot reconstruction surgery is an umbrella terms used for a variety of surgical procedures to repair the bones and tendons of the foot to restore the foot arch and reduce pain, correct deformities, and restore function.
Flatfoot reconstruction surgery is used for people that have a low foot arch and are experiencing symptoms such as pain and posture problems that are limiting their ability to function in daily life. In most cases, non-surgical methods have been tried but failed to help reduce symptoms.
How is Flatfoot surgery performed?
Depending on the cause of flatfoot, a combination of surgical techniques is used to restore the foot shape. Your orthopaedic specialist surgeon will discuss surgical options with you prior to undergoing any procedure.
Posterior Tibial Tendon Dysfunction (PTTD)
Posterior tibial tendon dysfunction (PTTD) is one of most common causes of acquired flatfoot in adults. The posterior tibial tendon connects the calf muscles of the leg to a bone in the foot arch called the navicular and weakening or problems with this tendon causes the foot to lose its shape and results in pain and swelling. The following procedures may be used in flatfoot caused by posterior tibial tendon dysfunction
Lengthening of the Achilles Tendon (Gastrocnemius Recession): This is used to lengthen and increase flexibility of the calf muscles. This prevents flatfoot for reoccurring and is useful to help patients that having difficulty lifting their ankles up. It is used in combination with other surgeries to repair flatfoot.
Cleaning the tendon (Tenosynovectomy): This surgery involves cleaning up the tendon by removing inflamed or damaged tendon tissue. It is used primarily for early and mild cases of flatfoot to reduce pain and swelling. Unfortunately, it carries the risk of the tendon continuing to degenerate and resurface of pain.
Tendon transfer: This procedure removes diseased or damaged tendon and replaces it with healthy tendon from another part of the foot to reform the foot arch. Tendon tissue that is not completely diseased may be preserved and attached to a healthy tendon.
Cutting and shifting bones (osteotomy): This procedure involves cutting and reconstructing the heel and midfoot bones to restore the foot arch. In more severe cases of flatfoot, bone from another area may be grafted to improve the structure of foot arch.
Subtalar implant: To repair the foot arch, a small titanium device is sometimes implanted into the side of the hindfoot.
Rheumatoid Arthritis
Flatfoot may be the result of rheumatoid arthritis which is a chronic inflammatory condition that affects the soft tissue of the foot and ankles. The loss of ligaments and cartilage causes pain and loss of structure in the foot. The following procedures may be used in flatfoot caused by rheumatoid arthritis:
· Fusion (arthrodesis): This procedure aims to fuse the joints of the foot to realign the bones and restore normal shape. During the surgery, joints affected by arthritis and all cartilage is removed and replaced with bone graft material to create a single solid bone structure. This eliminates any joint movements that causes arthritic pain. In most cases, fusion is used because arthritis has caused the foot to stiffen significantly that other surgical techniques cannot be used.
Injury or Trauma of the Foot
Ligaments of the foot provide structure and support to the foot arch. Damage or tear of these ligaments can cause the bones and joints to misalign and result in flattening of the foot arch. The following procedures may be used in flatfoot caused by injuries:
· Internal fixation: This procedure uses a combination of metal screws and plates to realign the bones of the foot.
Flatfoot surgery aims to restore the natural foot arch and relieve pain and posture issues.
What are some risks and complications of Flatfoot Surgery?
Before undergoing any surgery, an orthopaedic specialist surgeon will discuss risks and potential complications with you and answer any questions you might have.
Some risks include:
Wound infection: this occurs in less than 1% of all procedures and can be treated with antibiotics
Nerve damage: there is a small risk to losing sensation of the skin in area surrounding the surgical site, but this is very rare.
Blood clots: with any surgical procedure, there is a small risk of the blood clotting in the vessels causing pain and swelling. If you have known risk factors associated blood clots, the specialist may prescribe you with some blood-thinners during the recovery period. The risks are present but small. If you experience abnormal swelling and pain of the leg, please contact the specialist urgently.
Reappearance of symptoms: Although symptoms rarely continue after surgery, a small number of people may find that their pain and discomforts return. In this case, your specialist will discuss further treatment options with you. You may also have to use footwear insoles long-term.
How much does it cost to have Flatfoot surgery?
The costs to have Flatfoot surgery in Sydney depends on each individual treatment plan. Costs will depend on the treatment outcomes and complexity of the case presented. We provide full costs disclosure before initiating any treatments and therapies.
We accept most major private health insurance funding, and our knowledgeable staff can assist you with the health insurance claims process, but it is always helpful to contact your provider in advance to ensure that your insurance covers the orthopaedic procedure.
In most cases, you may be expected to pay a gap fee, but this is dependent on the cover of your private health insurance.
Associate Professor Roderick Kuo works only in the private health system and unfortunately does not maintain a public system list. However, some conditions may be treated with non-surgical methods such as physiotherapy that can be initiated after a consultation and review of your circumstances.
Here’s what to do next…
Research your condition and treatment options
We provide extensive information about Flatfoot on our conditions page.
Read our FAQ about Flatfoot Surgery below.
Do further research and contact us with any questions you may have.
Book a consultation with Associate Professor Roderick Kuo
Prior to your appointment, please obtain a referral from your General Practitioner. This will allow you to claim a Medicare rebate on the consultation fees.
Call or email our team at Specialty Orthopaedics to book your consultation.
Frequently Asked Questions about Flatfoot Surgery
-
You may be required to stay 1-2 days in hospital.
-
Prior to surgery, you will be given general anaesthesia and a local injection around the foot area, so you remain pain-free during and after the surgery. During the recovery period, you may be prescribed some stronger painkillers to reduce any discomforts. In the recovery and rehabilitation period, you may experience some discomforts, but this can be managed with painkillers.
-
After the surgery is complete, a plaster cast will be placed from foot to knee. Afterwards you will be sent to the recovery unit and monitored for a period of time to allow the general anaesthesia to wear off and your body vitals to normalise. It is important at this time to report any discomfort, pain, or nausea you may have to the doctors as they can assess your need for painkillers or anti-nausea drugs when you are discharged.
You will be referred to a physiotherapist who will start you on a recovery programme. It is recommended that you follow the guidance of the physiotherapy programme as it will speed up your recovery drastically and allow you to get back on your feet sooner.
-
In the first week after the surgery, you should attempt to minimalize moving around unless necessary. This is to ensure the foot structure is kept in place while healing. Avoid wear-bearing on the operated foot.
You should avoid taking any anti-inflammatory medication such as ibuprofen as this may interfere with the bone healing process.
Attempt to elevate your foot to the level of your heart to reduce swelling and take painkillers whenever you experience pain.
You may find some blood ooze at the site of the surgery which is normal. However, if you notice bleeding does not stop, please contact the orthopaedic specialist surgeon urgently.
-
For the first 6 weeks, you will have the foot in a plaster cast or boot, and you should NOT weight bear. You may move around with the use of crutches, frame or knee scooter.
After 6 weeks, if the foot has healed sufficiently, the boot/plaster cast will be removed, and you will be given a brace or footwear insoles. You should be able to weight-bear at this time and regain the ability to walk independently without assistive devices. You should consult with the orthopaedic specialist surgeon prior to removing the boot/plaster cast and attempting to weight-bear on the foot.
-
Healing and recovery times are different for each individual person. In general, you should be able to return to work in 2 weeks if you mostly sit at work. You should allow for 3-6 months to recover if your work involves manual labour.
-
The typical follow-up appoints after you have been discharged is as following:
10-14 days after surgery
At the first appointment, the orthopaedic specialist surgeon will remove your plaster casts and wound sutures. An X-ray will be ordered to check the progress of bone healing then you will be fitted with a new plaster cast or a boot.
Six weeks after surgery
At this appointment, the foot will be X-rayed, and the plaster casts or boot removed. You will be given insoles for your footwear and at this time you should be able to weight-bear on the foot.
Three months after surgery
The orthopaedic specialist surgeon will review your progress at this appointment. It is important to report how if you have any more pain or discomforts in your foot.
Six to twelve months after surgery
This will be the final appointment to review your progress. If all is well, you will be discharged. Occasionally you may require removal of any metal implants.
Important: Information is provided for guidance only. Individual circumstances may differ and the best way to approach a condition is by individual medical consultation where a specialist can tailor a treatment plan to suit your needs.
Edited by Dr Roderick Kuo
Last updated: 5/5/24